Marie Lynn Miranda, head of the Children’s Environmental Health Initiative at Duke, uses sophisticated modeling to tackle stubborn public-health problems.
Originally published in Duke Magazine.
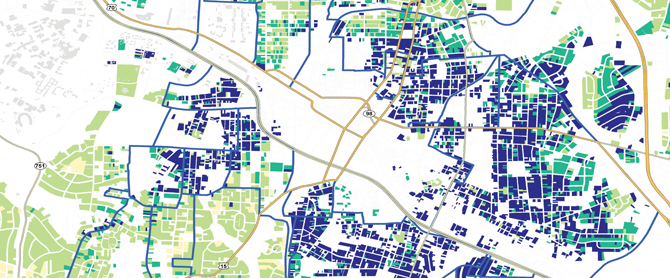
GIS data generate nuanced spatial analyses in this map of Durham neighborhoods; dark blue areas represent parcels at highest risk for lead-paint exposure, green parcels are at lower risk, and yellow parcels contain lowest risk.
LAST FALL, DURHAM COUNTY HEALTH DIRECTOR Gayle Harris faced a thorny question: How do you get a confused and suspicious public inoculated against H1N1 influenza? The much-feared flu strain had already arrived in Durham, forcing Duke to cancel several summer youth camps. Nationwide, H1N1 had infected 22 million people, killing 3,900, according to estimates by the U.S. Centers for Disease Control and Prevention. Still, persuading Durhamites to get vaccinated was proving tough.
“The H1N1 messaging from federal down to state came in bits and pieces,” Harris says. “First we said, ‘We have the outbreak, but we don’t have enough vaccine.’ Then we said, ‘Oh, we’ll let everybody have it. We have more than enough.’ What the public heard was: ‘We have something we don’t know how to deal with.’” What’s more, she says, certain populations appeared to be missing from the city’s vaccination clinics. As she visited clinics around the city, she noticed good numbers of Hispanics in the flu-shot lines, but very few African Americans.
Harris, who is African American, hypothesized that some black residents were suspicious of getting a live vaccine for a new strain. “Those people who have the memory of Tuskegee don’t want to be engaged with this experimental kind of thing,” she says, referring to an infamous forty-year research project in Tuskegee, Alabama, in which black men infected with syphilis unknowingly went untreated.
Harris didn’t want to rely solely on her own impressions. To reach those who needed the vaccine the most, she needed data—and she needed it fast. The health director turned to one of her most trusted colleagues, Marie Lynn Miranda ’85, director of the Children’s Environmental Health Initiative (CEHI), an interdisciplinary program housed at Duke’s Nicholas School of the Environment.
“Can you create a map for me showing the locations of Durham County residents who have presented in [local emergency rooms] with influenza-like illnesses?” Harris wrote Miranda in an e-mail message. “I would like to use it to help target locations for mass clinics.”
Miranda knew she could produce more than a simple map. CEHI’s forte is creating what’s called spatial data architecture—using Geographic Information Systems (GIS) to turn raw data into multilayered maps that reveal much more about a public-health problem than lower-tech tools can uncover by themselves. Miranda has used her mapping skills to tackle problems as widespread as childhood lead poisoning in Durham’s older neighborhoods; the rise in asthma rates after Hurricane Floyd; and the high rate of Lou Gehrig’s disease among some Gulf War veterans.
Miranda started with Duke’s patient database, which told her who had already sought treatment through the university’s health system for flu symptoms. “What became apparent was that we did not know where people who had been vaccinated lived relative to where people who were sick lived,” she says. The Durham County Health Department’s
immunization records were handwritten; its patient consent forms had not been computerized. Knowing that timeliness was crucial, Miranda hired six high-school students, trained them in medical privacy issues, and paid them to enter thousands of records into CEHI computers during their December holiday break.
The resulting maps showed that East Durham’s Fayetteville Street corridor, which is predominantly African American, had a particularly low immunization rate. Until then, most of the health department’s vaccination clinics were located in West Durham, where the population is whiter, and in the downtown commercial district. As soon as Harris reviewed the maps, she decided to match the geography to the need—and offer clinics in some of the most underserved areas, including a school and church in the Fayetteville Street corridor.
Moreover, Miranda’s mapping system provided a tool for the health department to improve its strategic planning in the future. The spatial data architecture now contains many layers of information: the locations of pediatric patients for whom influenza presents the greatest danger (children with asthma, for example); demographic information like race, age, sex, and neighborhood characteristics; and community resources like churches and schools, which show health planners where they can set up clinics. Knowing who’s getting sick and who’s not getting immunized will allow the health department to target the populations in greatest need during upcoming flu seasons.
“We need to reach out to those communities to say, ‘Help us understand what happened. Why did you not take advantage? What could we have done differently?’” Harris says.
OVER THE PAST DECADE, Miranda has become a national leader in using GIS technology to tackle complex public-health problems, particularly those affecting minorities and the poor. She does this not only by crunching data. She also works directly with community members to figure out how to use that data to meet their needs.
“She terms herself as a geek, but she is a very unusual geek,” says Harris, the county health director. “She is very much into social justice. She is passionate about what she does. In spite of her being highly intelligent and highly into technology, when she talks about it, she can put faces on it.”
Miranda does this work under the auspices of CEHI, the research, education, and outreach program she founded, which established partnerships with experts throughout the university. CEHI’s “most mature” project, as Miranda calls it, is designed to address lead exposure in children. Lead—found in paint, drinking water, and even soil tracked into homes—can cause brain damage, learning disabilities, behavior problems, and slowed growth. Children are particularly prone to its effects, both because they ingest paint in older houses and because their bodies absorb the element more easily. Children’s nervous systems are also more sensitive than adults’ to lead’s effects.
When they began working with CEHI researchers about ten years ago, Durham County health officials already knew that lead poisoning was a problem, especially in poorer communities. But “we had not done anything to go out and identify those kids who could be at risk,” Harris says. “We were just reacting to the ones that were diagnosed by physicians.” A citizen group called Durham CAN (Congregations, Associations and Neighborhoods) had been lobbying the department to address the issue more aggressively. But county officials said they lacked the money for universal screening and had no precise way to locate the children most in need of testing.
Maps that identified broad risk factors—the oldest houses or the poorest communities—wouldn’t add much value. “You see a lot of public-health data displayed with GIS these days,” Miranda says. “A lot of it is done at the county or ZIP code level. If I said to the director of the health department, ‘Boy, you really need to worry about ZIP code 27704,’ she would look at me and say, ‘Well, tell me something I don’t know already.’”
Instead, Miranda and her staff met with community leaders to find out what information would be most helpful. They then created a model that zoomed down to the level of individual properties. They introduced every possible variable that could influence lead exposure, whether the information existed at the level of an individual property or tax parcel (for example, tax value, year of construction, and owner vs. renter occupancy) or a block or group of blocks used for compiling census data (racial demographics, median family income, childhood poverty rate). CEHI also negotiated confidential access to lead-screening data: the addresses, ages, and blood levels of the youngsters who had been tested and whether their families qualified for Medicaid and WIC. Plugging these GIS data into a statistical program, Miranda and her staff calculated how much each factor actually influenced lead levels. They then transferred their findings back into the GIS program—and assigned a risk category to every one of Durham County’s 62,000 residential parcels.
In the resulting color-coded map, the most worrisome 10 percent of properties are shaded dark blue, the next 10 percent bright green, and so on. “So now, if the health director says to me, ‘I have the resources to screen 1,000 kids; where should I go?’ I don’t have to tell her, ‘Go to ZIP code 27704,’” Miranda says. “I can tell her, very specifically, ‘Go to these houses.’”
Not only that. The model can map the nearest facilities to set up community-based test sites. “You could say, ‘Here are all the churches where you can do blood-lead screening,’” says Miranda. “Or you could do it at the pharmacies. If you wanted me to map all the tiendas to reach the Hispanic community, well, I can map that for you.” The maps also make it possible to select houses for cleanup and to target communities for education.
After Durham County adopted CEHI’s model in 2002, according to its internal data, the detection rate for lead-poisoned children shot up 600 percent—“with a zero percent increase in cost,” Miranda says. Since then, CEHI has made its model available to groups in forty-three North Carolina counties, as well as some localities outside the state, including Kenosha County, Wisconsin, and Miranda’s hometown of Detroit.
CEHI went beyond identifying high-risk houses and possible clinic locations. For example, it plugged North Carolina’s end-of-grade test scores into it model, enabling researchers to study whether there’s an association between lead exposure and school performance. (There is.) And it used the technology to show that changes in water disinfection processes around Goldsboro, North Carolina, were associated with elevated bloodlead levels—perhaps owing to changes in the chemistry of the water running through lead pipes and fixtures. Both local and state officials have used CEHI’s technology to leverage more funding for lead programs.
Ed Norman, who runs North Carolina’s Childhood Lead Poisoning Prevention Program, says he’s not surprised by CEHI’s success. “The thing Marie Lynn has been able to do so effectively is take that kind of predictive model and make it useful to folks in the community that aren’t scientists—lay-persons or activists who want to see an improvement in the area of social justice. Marie Lynn is very committed to that. Everything she’s done is targeted in that way, but in a scientifically rigorous way.”
MIRANDA IS THE DAUGHTER OF IMMIGRANTS from Goa, a former Portuguese outpost on the West Coast of India, whose culture is part Asian, part Latin. Her father taught civil engineering at the University of Detroit. Despite her middle-class upbringing, “I always say that I came to my interest in environmental work through deprivation processes,” she says. “Detroit has always been a city that swings very, very hard with the automobile industry. Whenever the industry was doing poorly, crime went up, and the amenities that were available went down. What people’s houses looked like, and the number of houses that were for sale—you could just see the peaks and troughs in the economy.” Even during flush times, public facilities were lacking. Miranda learned to swim at Duke because, as a child, she had no access to a pool.
“Many people who work in the environment are especially interested in what I would call green issues, like biodiversity and species preservation,” Miranda says. “I am much more interested in brown issues: pollution exposures and chemical exposures, which we typically see in urban environments. Early on, I had a big interest in urban blight and its converse, urban renovation. Growing up in Detroit, we had race riots when I was a little girl. Then, by the time I was in high school, we had built the Renaissance Center down on the waterfront, and there was so much hope that that would be transformative. Now it’s hard when I am back working in Detroit: One out of every four houses is in foreclosure.”
Miranda’s upbringing also shaped her interest in minority issues. She lived in a neighborhood that had become mostly African American during her adolescence and attended, on scholarship, an overwhelmingly white Catholic high school. In both worlds, she was a minority. “I’m not white, and I’m not black. And at that time, we didn’t really talk about brown people,” she says. Growing up in Detroit “gave me an understanding and an interest in the experience of all minorities in the U.S. I had this opportunity to figure out how to navigate successfully with a lot of different cultures. I always liked learning about all that stuff.”
Miranda studied mathematics and economics at Duke (where she was also one of several student managers of the men’s basketball team) and then earned a Ph.D. in economics at Harvard University. She considered working for the World Bank or the nonprofit Resources for the Future, both of which eventually offered her jobs. But her dissertation adviser at Harvard, C. Peter Timmer (now a professor emeritus of development studies), had a hunch she’d be a good educator and encouraged her to teach a class. “Twenty minutes into the first session, I thought to myself, I love the classroom,” she says.
When Miranda joined the Duke faculty in 1990, she was interested primarily in land-management issues. That interest didn’t sustain her, though. “Scientifically, I really like thinking about the biological pathways by which these environmental factors become important. I’m interested in both the biological and the social pathways. And in the land-management work, it’s mostly about the social pathways”—for example, what happens when newcomers move into a village with strong cultural traditions limiting how much timber residents can remove from the forest or the number of privately owned livestock allowed to graze on public lands.
Becoming the mother of three clarified her professional ambitions. “It’s a pretty high bar,” she says. “Every hour that I spend at work is an hour that I don’t have with my children. I need that work to be very meaningful.” Focusing on children’s health, she says, “meant that I was doing the same thing at work and at home, which was trying to create an environment where children can prosper.”
Venturing into human health meant teaching herself toxicology—reading extensively and asking “endless questions” of Nicholas School colleagues. (Richard Di Giulio, a professor of environmental toxicology, periodically tells her, “You know more about receptor biology than any economist I’ve ever met.”) In 1998, Miranda formalized her interest by starting the Children’s Environmental Health Initiative.
FROM THE START, CEHI’S GOAL has been to turn the usual crisis driven approach to public health upside down. “The standard operating paradigm is that we wait for kids to get sick, and then we go into their homes, their daycare centers, their grandmas’ homes, their schools, and try to figure out what made them sick,” Miranda says. This is true of medicine more generally, she says: In part because of insurance payment rules and inadequate technology, patients often don’t get the preventive care they need. “What we’re interested in doing is trying to use these advanced information technologies to identify the places that are likely to have adverse impacts on children or pregnant women and then push some policy levers to effect change.” Much of what she does can be described as “translational medicine”: making sure advances in research actually reach the populations most affected by the issue.
Over the past few years, CEHI has expanded its scope well beyond lead exposure. For example, Miranda worries that some youngsters start their lives—literally from day one or earlier—at high risk for illness and learning problems. This includes children who are born prematurely or at lower-than normal weights. Non-Hispanic black women suffer an unusually high rate of pregnancy problems, for reasons that are not clear. Poverty can’t be the sole cause, Miranda says, because equally impoverished Hispanics typically have fewer problems. Nor is lack of prenatal care entirely responsible. “We’ve spent a lot of money improving access to care, and we haven’t really narrowed the gap,” she says.
In 2007, CEHI secured $7.7 million from the U.S. Environmental Protection Agency to launch the Southern Center on Environmentally-Driven Disparities in Birth Outcomes (SCEDDBO), one of eleven federally funded Children’s Centers around the country. SCEDDBO brings together collaborators from across campus—including the Sanford School of Public Policy, the medical center, the department of statistical science, and the Center for Human Genetics—to study how a wide variety of factors influence fetal and infant development.
SCEDDBO runs three projects: examining all North Carolina birth records since 1978 (and cross-referencing birth locations with such data as air-pollution levels, water-quality tests, and landfill locations) to find links between environmental contamination and pregnancy problems; surveying 1,800 pregnant women who use Durham obstetric clinics about their toxic exposures and social stressors, testing them for genetic vulnerabilities, then following their pregnancy outcomes; and studying what happens to mice exposed to certain air pollutants during and after pregnancy.
These projects are all integrated, Miranda notes. For example, data from the mouse research might help explain the biological pathways for trends spotted in the birth-records study. “This is why we collaborate with people from a lot of different fields,” she says. The results of one project might lead investigators to rethink how they approach the other two—“a huge feedback loop,” Miranda calls it. This is particularly useful for looking at health problems with myriad possible risk factors and figuring out which of those factors are truly causal and which are simply coincidental. “In public health,” she says, “the simple questions were answered a while ago. Now we’re left with really hard questions, and they require integrated approaches.” One conclusion already apparent from SCEDDBO’s work, Miranda says: “Even in North Carolina, which generally is in compliance with the federal air-quality standards, we see a clear association between exposure to particulate matter and poorer birth outcomes.”
In another effort, which Miranda presented to National Institutes of Health director Francis Collins when he visited Duke in May, CEHI is working with the Duke University Health System to superimpose geographic information on patient records. Merging these two types of data, she says, could have numerous uses. For example, it could allow doctors to help their sedentary patients get more exercise by offering them safe and useful walking routes near their homes. Or it could help researchers analyze whether patients who routinely use emergency rooms tend to live in neighborhoods that lack bus transportation to walk-in clinics. Miranda acknowledges that the “C” in CEHI might eventually need revisiting. But she adds, “We all feel such deep attachment to [children’s health] that we seem to be incapable of making that transition.”
To watch Miranda interact with the children whose health she studies is to forget that she spends much of her time in the world of statistics, medical records, and flat-screen monitors. On a Friday morning this past spring, Miranda and her staff distributed books to seventy-two preschoolers at the Operation Breakthrough Head Start center in downtown Durham.
This was not a feel-good exercise. Research shows that introducing even a small amount of age-appropriate literature into disadvantaged homes can substantially improve school success. Yet working at Durham clinics, “we were seeing households where there were literally no children’s books,” says Miranda, whose own children have hundreds of books. “We said, ‘Golly, this seems like something we can address.’” After raising money from foundations and individual donors, and negotiating discounts from publishers, CEHI purchased enough books in 2009 to give three volumes to every Head Start student in Durham County. This year, the program expanded to include nearby Orange County as well.
The four- and five-year-olds had assembled in Operation Breakthrough’s concrete courtyard. “Good morning,” said Miranda, looking as wiggly as the kids. She led them in neck stretches and shoulder rolls before settling them down and introducing herself. “There are three things in the world I really love,” she told them. “The first one is my family.” She asks the kids to guess the second. “I’ll give you a hint: There’s a lot of them in front of me right now.”
“Children!” came the collective cry.
“What do think the third thing in my very, very favorite list is?”
“Books?” a child ventured.
“Oh my goodness!” she said. “You guessed it on the very first guess! If there’s a lot of children here, what do you think I need?”
“A lot of books!”
Soon CEHI’s staff members were handing out seventy-two string backpacks, each containing three award-winning books tailored to the students’ home languages. The Duke employees led a song about reading, accompanied by a little dance. Breaking from the adults, Miranda jumped into the pack of children and playfully tapped out a rhythm on the shoulders of the boy dancing in front of her. Finally, as the classes adjourned—to listen as CEHI staffers read Click, Clack, Moo: Cows That Type—Miranda stood in the doorway to high-five each child. “Oh! Yes! Yes!” she shouted. “These children are ready to read.”
Miranda gets most excited about the work she does off campus. Likewise, her colleagues talk enthusiastically about her outreach abilities. By engaging the community, she’s not only acting with a conscience, she’s also gathering better data. “When you are doing environmental epidemiology research, we now know that you cannot do that work adequately unless you involve a community,” says Linda Birnbaum, director of NIH’s National Institute of Environmental Health Sciences. “You can’t go in and say, ‘We’re going to study you.’ You’re not going to get the information, the participation that you need to do the study. Marie Lynn is one of the people who actually pioneered some of this—going in, meeting with the organizers in the community, and getting them involved from the very beginning. She wasn’t the first, but she was instrumental in demonstrating its importance.”
Harris, the Durham County health director, recalls working with Miranda on Durham Health Innovations, a Duke-Durham partnership focused on conditions that are prevalent in the county but inefficiently treated and prevented, including asthma, HIV, and substance abuse. Harris was struck by how attuned Miranda was to community representatives who might not understand policy details. “Marie Lynn made it her job to make sure that what was being said was not in acronyms or jargon,” Harris says. “She always would say, ‘Hold it. Are you with us here?’ It wasn’t in a condescending manner. It was in a manner to say, ‘I want you to be included in this, so that you can make the decisions that need to be made.’”
“She’s almost like translational medicine itself,” Harris says. “She is small in stature, but the shadow that she casts is huge.”
Postscript: Miranda is now dean of the School of Natural Resources and Environment at the University of Michigan.




